Portal:Medicine
The Medicine Portal

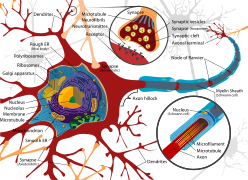
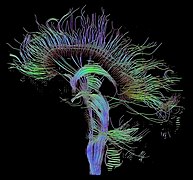
Medicine is the science and practice of caring for patients, managing the diagnosis, prognosis, prevention, treatment, palliation of their injury or disease, and promoting their health. Medicine encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness. Contemporary medicine applies biomedical sciences, biomedical research, genetics, and medical technology to diagnose, treat, and prevent injury and disease, typically through pharmaceuticals or surgery, but also through therapies as diverse as psychotherapy, external splints and traction, medical devices, biologics, and ionizing radiation, amongst others.
Medicine has been practiced since prehistoric times, and for most of this time it was an art (an area of creativity and skill), frequently having connections to the religious and philosophical beliefs of local culture. For example, a medicine man would apply herbs and say prayers for healing, or an ancient philosopher and physician would apply bloodletting according to the theories of humorism. In recent centuries, since the advent of modern science, most medicine has become a combination of art and science (both basic and applied, under the umbrella of medical science). For example, while stitching technique for sutures is an art learned through practice, knowledge of what happens at the cellular and molecular level in the tissues being stitched arises through science.
Prescientific forms of medicine, now known as traditional medicine or folk medicine, remain commonly used in the absence of scientific medicine and are thus called alternative medicine. Alternative treatments outside of scientific medicine with ethical, safety and efficacy concerns are termed quackery. (Full article...)
-
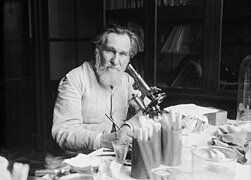
Howard Walter Florey, Baron Florey, OM FRS FRCP (/ˈflɔːri/; 24 September 1898 – 21 February 1968) was an Australian pharmacologist and pathologist who shared the Nobel Prize in Physiology or Medicine in 1945 with Ernst Chain and Sir Alexander Fleming for his role in the development of penicillin.
Although Fleming received most of the credit for the discovery of penicillin, it was Florey and his team at the University of Oxford who made it into a useful and effective drug, ten years after Fleming had abandoned its development. They developed techniques for growing, purifying and manufacturing the drug, tested it for toxicity and efficacy on animals, and carried out the first clinical trials. In 1941, they used it to treat a police constable from Oxford. He started to recover, but subsequently died because Florey was unable, at that time, to make enough penicillin. Later trials in Britain, the United States and North Africa were highly successful. (Full article...) -
Chagas disease, also known as American trypanosomiasis, is a tropical parasitic disease caused by Trypanosoma cruzi. It is spread mostly by insects in the subfamily Triatominae, known as "kissing bugs". The symptoms change over the course of the infection. In the early stage, symptoms are typically either not present or mild, and may include fever, swollen lymph nodes, headaches, or swelling at the site of the bite. After four to eight weeks, untreated individuals enter the chronic phase of disease, which in most cases does not result in further symptoms. Up to 45% of people with chronic infections develop heart disease 10–30 years after the initial illness, which can lead to heart failure. Digestive complications, including an enlarged esophagus or an enlarged colon, may also occur in up to 21% of people, and up to 10% of people may experience nerve damage.
T. cruzi is commonly spread to humans and other mammals by the kissing bug's bite wound and the bug's infected feces. The disease may also be spread through blood transfusion, organ transplantation, consuming food or drink contaminated with the parasites, and vertical transmission (from a mother to her baby). Diagnosis of early disease is by finding the parasite in the blood using a microscope or detecting its DNA by polymerase chain reaction. Chronic disease is diagnosed by finding antibodies for T. cruzi in the blood. (Full article...) -
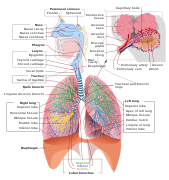
Oxygen toxicity is a condition resulting from the harmful effects of breathing molecular oxygen (O
2) at increased partial pressures. Severe cases can result in cell damage and death, with effects most often seen in the central nervous system, lungs, and eyes. Historically, the central nervous system condition was called the Paul Bert effect, and the pulmonary condition the Lorrain Smith effect, after the researchers who pioneered the discoveries and descriptions in the late 19th century. Oxygen toxicity is a concern for underwater divers, those on high concentrations of supplemental oxygen, and those undergoing hyperbaric oxygen therapy.
The result of breathing increased partial pressures of oxygen is hyperoxia, an excess of oxygen in body tissues. The body is affected in different ways depending on the type of exposure. Central nervous system toxicity is caused by short exposure to high partial pressures of oxygen at greater than atmospheric pressure. Pulmonary and ocular toxicity result from longer exposure to increased oxygen levels at normal pressure. Symptoms may include disorientation, breathing problems, and vision changes such as myopia. Prolonged exposure to above-normal oxygen partial pressures, or shorter exposures to very high partial pressures, can cause oxidative damage to cell membranes, collapse of the alveoli in the lungs, retinal detachment, and seizures. Oxygen toxicity is managed by reducing the exposure to increased oxygen levels. Studies show that, in the long term, a robust recovery from most types of oxygen toxicity is possible. (Full article...) -
Leeches are segmented parasitic or predatory worms that comprise the subclass Hirudinea within the phylum Annelida. They are closely related to the oligochaetes, which include the earthworm, and like them have soft, muscular segmented bodies that can lengthen and contract. Both groups are hermaphrodites and have a clitellum, but leeches typically differ from the oligochaetes in having suckers at both ends and in having ring markings that do not correspond with their internal segmentation. The body is muscular and relatively solid, and the coelom, the spacious body cavity found in other annelids, is reduced to small channels.
The majority of leeches live in freshwater habitats, while some species can be found in terrestrial or marine environments. The best-known species, such as the medicinal leech, Hirudo medicinalis, are hematophagous, attaching themselves to a host with a sucker and feeding on blood, having first secreted the peptide hirudin to prevent the blood from clotting. The jaws used to pierce the skin are replaced in other species by a proboscis which is pushed into the skin. A minority of leech species are predatory, mostly preying on small invertebrates. (Full article...) -
Helium (from Greek: ἥλιος, romanized: helios, lit. 'sun') is a chemical element; it has symbol He and atomic number 2. It is a colorless, odorless, tasteless, non-toxic, inert, monatomic gas and the first in the noble gas group in the periodic table. Its boiling point is the lowest among all the elements, and it does not have a melting point at standard pressures. It is the second-lightest and second most abundant element in the observable universe, after hydrogen. It is present at about 24% of the total elemental mass, which is more than 12 times the mass of all the heavier elements combined. Its abundance is similar to this in both the Sun and Jupiter, because of the very high nuclear binding energy (per nucleon) of helium-4, with respect to the next three elements after helium. This helium-4 binding energy also accounts for why it is a product of both nuclear fusion and radioactive decay. The most common isotope of helium in the universe is helium-4, the vast majority of which was formed during the Big Bang. Large amounts of new helium are created by nuclear fusion of hydrogen in stars.
Helium was first detected as an unknown, yellow spectral line signature in sunlight during a solar eclipse in 1868 by Georges Rayet, Captain C. T. Haig, Norman R. Pogson, and Lieutenant John Herschel, and was subsequently confirmed by French astronomer Jules Janssen. Janssen is often jointly credited with detecting the element, along with Norman Lockyer. Janssen recorded the helium spectral line during the solar eclipse of 1868, while Lockyer observed it from Britain. However, only Lockyer proposed that the line was due to a new element, which he named after the Sun. The formal discovery of the element was made in 1895 by chemists Sir William Ramsay, Per Teodor Cleve, and Nils Abraham Langlet, who found helium emanating from the uranium ore cleveite, which is now not regarded as a separate mineral species, but as a variety of uraninite. In 1903, large reserves of helium were found in natural gas fields in parts of the United States, by far the largest supplier of the gas today. (Full article...) -
Dementia with Lewy bodies (DLB) is a type of dementia characterized by changes in sleep, behavior, cognition, movement, and regulation of automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive impairment interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described on autopsy by Kenji Kosaka in 1976, and he named the condition several years later.
REM sleep behavior disorder (RBD)—in which people lose the muscle paralysis (atonia) that normally occurs during REM sleep and act out their dreams—is a core feature. RBD may appear years or decades before other symptoms. Other core features are visual hallucinations, marked fluctuations in attention or alertness, and parkinsonism (slowness of movement, trouble walking, or rigidity). A presumptive diagnosis can be made if several disease features or biomarkers are present; the diagnostic workup may include blood tests, neuropsychological tests, imaging, and sleep studies. A definitive diagnosis usually requires an autopsy. (Full article...) -
Brigadier Sir Neil Hamilton Fairley, KBE, CStJ, FRACP, FRCP, FRCPE, FRS (15 July 1891 – 19 April 1966) was an Australian physician, medical scientist, and army officer who was instrumental in saving thousands of Allied lives from malaria and other diseases.
A graduate of the University of Melbourne, where he was resident of Ormond College, Fairley joined the Australian Army Medical Corps in 1915. He investigated an epidemic of meningitis that was occurring in Army camps in Australia. While with the 14th General Hospital in Cairo, he investigated schistosomiasis (then known as bilharzia) and developed tests and treatments for the disease. In the inter-war period he became renowned as an expert on tropical medicine. (Full article...) -
Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of pancreatic cancer are known.
The most common, pancreatic adenocarcinoma, accounts for about 90% of cases, and the term "pancreatic cancer" is sometimes used to refer only to that type. These adenocarcinomas start within the part of the pancreas that makes digestive enzymes. Several other types of cancer, which collectively represent the majority of the non-adenocarcinomas, can also arise from these cells. (Full article...) -
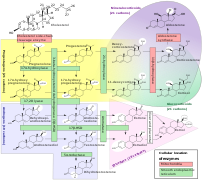
Ray Fletcher Farquharson MBE (4 August 1897 – 1 June 1965) was a Canadian medical doctor, university professor, and medical researcher. Born in Claude, Ontario, he attended and taught at the University of Toronto for most of his life, and was trained and employed at Toronto General Hospital. With co-researcher Arthur Squires, Farquharson was responsible for the discovery of the Farquharson phenomenon, an important principle of endocrinology, which is that administering external hormones suppresses the natural production of that hormone.
He served in the First and Second World Wars, earning appointment as a Member of the Order of the British Empire for his medical work during the latter. He chaired the Penicillin Committee of Canada and served as a medical consultant for the Royal Canadian Air Force. He was awarded the Queen's Coronation Medal in 1953 for his work for the Defence Review Board. Farquharson was also a charter member of the Royal College of Physicians and Surgeons of Canada. (Full article...) -
Osteochondritis dissecans (OCD or OD) is a joint disorder primarily of the subchondral bone in which cracks form in the articular cartilage and the underlying subchondral bone. OCD usually causes pain during and after sports. In later stages of the disorder there will be swelling of the affected joint which catches and locks during movement. Physical examination in the early stages does only show pain as symptom, in later stages there could be an effusion, tenderness, and a crackling sound with joint movement.
OCD is caused by blood deprivation of the secondary physes around the bone core of the femoral condyle. This happens to the epiphyseal vessels under the influence of repetitive overloading of the joint during running and jumping sports. During growth such chondronecrotic areas grow into the subchondral bone. There it will show as bone defect area under articular cartilage. The bone will then possibly heal to the surrounding condylar bone in 50% of the cases. Or it will develop into a pseudarthrosis between condylar bone core and osteochondritis flake leaving the articular cartilage it supports prone to damage. The damage is executed by ongoing sport overload. The result is fragmentation (dissection) of both cartilage and bone, and the free movement of these bone and cartilage fragments within the joint space, causing pain, blockage and further damage. OCD has a typical anamnesis with pain during and after sports without any history of trauma. Some symptoms of late stages of osteochondritis dissecans are found with other diseases like rheumatoid disease of children and meniscal ruptures. The disease can be confirmed by X-rays, computed tomography (CT) or magnetic resonance imaging (MRI) scans. (Full article...) -
Race Against Time: Searching for Hope in AIDS-Ravaged Africa is a non-fiction book written by Stephen Lewis for the Massey Lectures. Lewis wrote it in early to mid-2005 and House of Anansi Press released it as a corresponding lecture series began in October 2005. Each of the book's chapters were delivered as a different lecture in a different Canadian city, beginning in Vancouver on October 18 and ending in Toronto on October 28. The speeches were aired on CBC Radio One between November 7 and 11. The author and orator, Stephen Lewis, was at that time the United Nations Special Envoy for HIV/AIDS in Africa and former Canadian ambassador to the United Nations. Although he wrote the book and lectures in his role as a concerned Canadian citizen, his criticism of the United Nations (UN), international organizations, and other diplomats, including naming specific people, was called undiplomatic and led several reviewers to speculate whether he would be removed from his UN position.
In the book and the lectures, Lewis argues that significant changes are required to meet the Millennium Development Goals in Africa by their 2015 deadline. Lewis explains the historical context of Africa since the 1980s, citing a succession of disastrous economic policies by international financial institutions that contributed to, rather than reduced, poverty. He connects the structural adjustment loans, with conditions of limited public spending on health and education infrastructure, to the uncontrolled spread of AIDS and subsequent food shortages as the disease infected much of the working-age population. Lewis also addresses such issues as discrimination against women and primary education for children. To help alleviate problems, he ends with potential solutions which mainly require increased funding by G8 countries to levels beyond what they promise. (Full article...) -
John Rolph (4 March 1793 – 19 October 1870) was a Canadian physician, lawyer, and political figure. As a politician, he was considered the leader of the Reform faction in the 1820s and helped plan the Upper Canada Rebellion. As a doctor, he founded several medical schools and incorporated new teaching techniques and medical procedures into his lectures. However, his actions against rival medical schools decreased public confidence in the ability of medical professionals to regulate themselves.
Rolph grew up in Thornbury, Gloucestershire, and was educated in medicine and law. He immigrated to Upper Canada in 1813 and lived on his father's farm in Port Talbot, where he practised law and medicine concurrently and opened a medical school called the Talbot Dispensary. In 1824, Rolph was elected to the Parliament of Upper Canada and returned to England to petition the Colonial Office to allow the naturalization of American citizens in Canada. He was elected as an alderman to Toronto's first city council, though he resigned after his council colleagues did not select him to be the city's mayor. (Full article...) -
In the early 20th century, German researchers found additional evidence linking smoking to health harms, which strengthened the anti-tobacco movement in the Weimar Republic and led to a state-supported anti-smoking campaign. Early anti-tobacco movements grew in many nations from the middle of the 19th century. The 1933–1945 anti-tobacco campaigns in Nazi Germany have been widely publicized, although stronger laws than those passed in Germany were passed in some American states, the UK, and elsewhere between 1890 and 1930. After 1941, anti-tobacco campaigns were restricted by the Nazi government.
The German movement was the most powerful anti-smoking movement in the world during the 1930s and early 1940s. However, tobacco control policy was incoherent and ineffective, with uncoordinated and often regional efforts by many actors. Obvious measures were not taken, and existing measures were not enforced. Some Nazi leaders condemned smoking and several of them openly criticized tobacco consumption, but others publicly smoked and denied that it was harmful. (Full article...) -
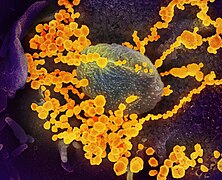
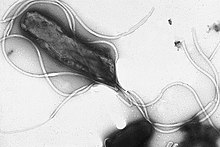
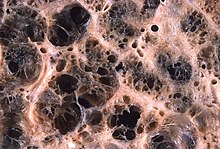
Helicobacter pylori, previously known as Campylobacter pylori, is a gram-negative, flagellated, helical bacterium. Mutants can have a rod or curved rod shape, and these are less effective. Its helical body (from which the genus name, Helicobacter, derives) is thought to have evolved in order to penetrate the mucous lining of the stomach, helped by its flagella, and thereby establish infection. The bacterium was first identified as the causal agent of gastric ulcers in 1983 by the Australian doctors Barry Marshall and Robin Warren, who obtained the Nobel prize in Medicine for this discovery.
Infection of the stomach with H. pylori is not the cause of illness itself; over half of the global population is infected but most are asymptomatic. Persistent colonization with more virulent strains can induce a number of gastric and extragastric disorders. Gastric disorders due to infection begin with gastritis, inflammation of the stomach lining. When infection is persistent the prolonged inflammation will become chronic gastritis. Initially this will be non-atrophic gastritis, but damage caused to the stomach lining can bring about the change to atrophic gastritis, and the development of ulcers both within the stomach itself or in the duodenum, the nearest part of the intestine. At this stage the risk of developing gastric cancer is high. However, the development of a duodenal ulcer has a lower risk of cancer.Helicobacter pylori is a class 1 carcinogen, and potential cancers include gastric mucosa-associated lymphoid tissue (MALT) lymphomas and gastric cancer. Infection with H. pylori is responsible for around 89 per cent of all gastric cancers, and is linked to the development of 5.5 per cent of all cases of cancer worldwide. H. pylori is the only bacterium known to cause cancer. (Full article...) -
Lung cancer, also known as lung carcinoma, is a malignant tumor that begins in the lung. Lung cancer is caused by genetic damage to the DNA of cells in the airways, often caused by cigarette smoking or inhaling damaging chemicals. Damaged airway cells gain the ability to multiply unchecked, causing the growth of a tumor. Without treatment, tumors spread throughout the lung, damaging lung function. Eventually lung tumors metastasize, spreading to other parts of the body.
Early lung cancer often has no symptoms and can only be detected by medical imaging. As the cancer progresses, most people experience nonspecific respiratory problems: coughing, shortness of breath, or chest pain. Other symptoms depend on the location and size of the tumor. Those suspected of having lung cancer typically undergo a series of imaging tests to determine the location and extent of any tumors. Definitive diagnosis of lung cancer requires a biopsy of the suspected tumor be examined by a pathologist under a microscope. In addition to recognizing cancerous cells, a pathologist can classify the tumor according to the type of cells it originates from. Around 15% of cases are small-cell lung cancer (SCLC), and the remaining 85% (the non-small-cell lung cancers or NSCLC) are adenocarcinomas, squamous-cell carcinomas, and large-cell carcinomas. After diagnosis, further imaging and biopsies are done to determine the cancer's stage based on how far it has spread. (Full article...)
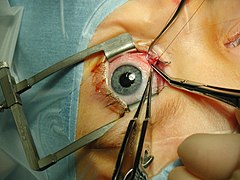
Selected image –

Photo credit: Original uploader was KieranMaher at en.wikibooks
WikiProject
Get involved by joining WikiProject Medicine. We discuss collaborations and all manner of issues on our talk page.
Related portals
-
Vertebral artery dissection (VAD) is a flap-like tear of the inner lining of the vertebral artery, which is located in the neck and supplies blood to the brain. After the tear, blood enters the arterial wall and forms a blood clot, thickening the artery wall and often impeding blood flow. The symptoms of vertebral artery dissection include head and neck pain and intermittent or permanent stroke symptoms such as difficulty speaking, impaired coordination, and visual loss. It is usually diagnosed with a contrast-enhanced CT or MRI scan.
Vertebral dissection may occur after physical trauma to the neck, such as a blunt injury (e.g. traffic collision), or strangulation, or after sudden neck movements, i.e. coughing, but may also happen spontaneously. 1–4% of spontaneous cases have a clear underlying connective tissue disorder affecting the blood vessels. Treatment is usually with either antiplatelet drugs such as aspirin or with anticoagulants such as heparin or warfarin. (Full article...) -
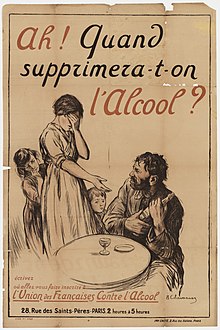
Alcoholism is the continued drinking of alcohol despite it causing problems. Some definitions require evidence of dependence and withdrawal. Problematic use of alcohol has been mentioned in the earliest historical records. The World Health Organization (WHO) estimated there were 283 million people with alcohol use disorders worldwide . The term alcoholism was first coined in 1852, but alcoholism and alcoholic are sometimes considered stigmatizing and to discourage seeking treatment, so diagnostic terms such as alcohol use disorder or alcohol dependence are often used instead in a clinical context.
Alcohol is addictive, and heavy long-term alcohol use results in many negative health and social consequences. It can damage all the organ systems, but especially affects the brain, heart, liver, pancreas and immune system. Heavy alcohol usage can result in trouble sleeping, and severe cognitive issues like dementia, brain damage, or Wernicke–Korsakoff syndrome. Physical effects include irregular heartbeat, an impaired immune response, liver cirrhosis, increased cancer risk, and severe withdrawal symptoms if stopped suddenly. These health effects can reduce life expectancy by 10 years. Drinking during pregnancy may harm the child's health, and drunk driving increases the risk of traffic accidents. Alcoholism is also associated with increases in violent and non-violent crime. While alcoholism directly resulted in 139,000 deaths worldwide in 2013, in 2012 3.3 million deaths may be attributable globally to alcohol. (Full article...) -

Colonel Sir Edward Ford, OBE, FRACP, FRCP (15 April 1902 – 27 August 1986) was an Australian soldier, academic and physician. He played an important role in the anti-malaria campaign in the South West Pacific Area during the Second World War, and in preventative medicine in Australia after the war, but is best known for his Bibliography of Australian Medicine.
After the war, Ford wrote a thesis on malaria control in the South West Pacific, for which he was awarded his Doctor of Medicine (MD) degree by the University of Melbourne in 1946. He became Director of the School of Public Health and Tropical Medicine at the University of Sydney in 1946, and Professor of Preventive Medicine in 1947, concurrently holding these two positions until his 1968 retirement. (Full article...) -

Hypericum perforatum, commonly known as St John's wort (sometimes perforate St John's wort or common St John's wort), is a flowering plant in the family Hypericaceae. It is a perennial plant that grows up to one meter tall, with many yellow flowers that have clearly visible black glands around their edges, long stamens (male reproductive organs), and three pistils (female reproductive organs). Probably a hybrid between the closely related H. attenuatum and H. maculatum (imperforate St John's wort) that originated in Siberia, the species is now found worldwide. It is native to temperate regions across Eurasia and North Africa, and has been introduced to East Asia, Australia, New Zealand, and parts of North and South America. In many areas where it is not native, H. perforatum is considered a noxious weed. It densely covers open areas to the exclusion of native plants, and is poor grazing material. As such, methods for biocontrol have been introduced in an attempt to slow or reverse the spread of the species.
The species produces numerous chemical compounds that are highly active. These chemicals are harmful to large animals, especially sheep, and help to deter herbivores from consuming the plant. Other chemicals in the plant, such as hypericin and hyperforin, have various uses in medicine. St John's wort has been used in traditional medicine since at least the first century AD, often as a cure-all or panacea. The oil from its glands can be extracted, or its above-ground parts can be ground into a powder called herba hyperici. In modern times, its use as an antidepressant has been the focus of numerous studies and clinical trials; however, the active ingredients can be very harmful or even lethal when taken alongside other medicines. (Full article...) -
International emergency medicine is a subspecialty of emergency medicine that focuses not only on the global practice of emergency medicine but also on efforts to promote the growth of emergency care as a branch of medicine throughout the world. The term international emergency medicine generally refers to the transfer of skills and knowledge—including knowledge of ambulance operations and other aspects of prehospital care—from developed emergency medical systems (EMSs) to those systems which are less developed. However, this definition has been criticized as oxymoronic, given the international nature of medicine and the number of physicians working internationally. From this point of view, international emergency medicine is better described as the training required for and the reality of practicing the specialty outside of one's native country.
Emergency medicine has been a recognized medical specialty in the United States and other developed countries for nearly forty years, although these countries' EMSs did not become fully mature until the early 1990s. At that point, some of its practitioners turned their attention from developing the specialty at home to developing it abroad, leading to the birth of international emergency medicine. They began to support the growth of emergency medicine worldwide, doing so through conferences, national and regional emergency medicine organizations, relief and development organizations, international emergency medicine fellowships, physician exchanges, information transfer, and curriculum development. (Full article...) -
Obesity hypoventilation syndrome (OHS) is a condition in which severely overweight people fail to breathe rapidly or deeply enough, resulting in low oxygen levels and high blood carbon dioxide (CO2) levels. The syndrome is often associated with obstructive sleep apnea (OSA), which causes periods of absent or reduced breathing in sleep, resulting in many partial awakenings during the night and sleepiness during the day. The disease puts strain on the heart, which may lead to heart failure and leg swelling.
Obesity hypoventilation syndrome is defined as the combination of obesity and an increased blood carbon dioxide level during the day that is not attributable to another cause of excessively slow or shallow breathing. (Full article...) -

Psychedelic music (sometimes called psychedelia) is a wide range of popular music styles and genres influenced by 1960s psychedelia, a subculture of people who used psychedelic drugs such as DMT, LSD, mescaline, and psilocybin mushrooms, to experience synesthesia and altered states of consciousness. Psychedelic music may also aim to enhance the experience of using these drugs and has been found to have a significant influence on psychedelic therapy.
Psychedelia embraces visual art, movies, and literature, as well as music. Psychedelic music emerged during the 1960s among folk and rock bands in the United States and the United Kingdom, creating the subgenres of psychedelic folk, psychedelic rock, acid rock, and psychedelic pop before declining in the early 1970s. Numerous spiritual successors followed in the ensuing decades, including progressive rock, krautrock, and heavy metal. Since the 1970s, revivals have included psychedelic funk, neo-psychedelia, and stoner rock as well as psychedelic electronic music genres such as acid house, trance music, and new rave. (Full article...) -
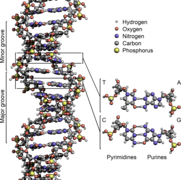
Beck–Fahrner syndrome, also known as BEFAHRS and TET3 deficiency, is a rare genetic disorder caused by mutations of the TET3 gene. The clinical presentation varies among individuals, but typically includes global developmental delay, slow progress in mental and physical activities, autism, decreased muscle tone, epilepsy and dysmorphic features.
Mutations in the TET3 gene disrupt DNA demethylation during embryogenesis, an essential epigenetic process contributing to the early development of the nervous system. They can occur from new genetic mutations or be inherited in an autosomal dominant manner. Diagnosis involves molecular and genetic testing in the context of typical symptoms. Management is supportive, aimed at improving quality of life. As of 2023, approximately 50 individuals have been diagnosed with Beck–Fahrner syndrome. (Full article...) -
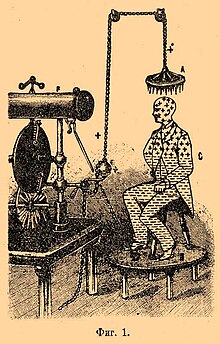
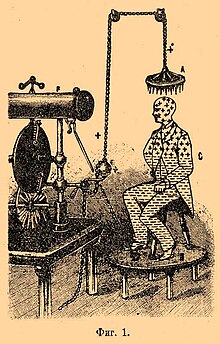
High voltage electric bath c. 1890s–1900s
An electric bath is a 19th-century medical treatment in which high-voltage electrical apparatus was used for electrifying patients by causing an electric charge to build up on their bodies. In the US this process was known as Franklinization after Benjamin Franklin. The process became widely known after Franklin described it in the mid-18th century, but after that it was mostly practiced by quacks. Golding Bird brought it into the mainstream at Guy's Hospital in the mid-19th century and it fell into disuse in the early 20th century. (Full article...) -
Dorothy P. Rice (June 11, 1922 – February 25, 2017) was an American health statistician whose work contributed to the creation of Medicare in the United States. Rice graduated from the University of Wisconsin–Madison and began working with the US government soon after, but left the workforce to begin raising a child. Just over a decade later, she returned to government work with a position at the Social Security Administration, where she was one of the first scientists to study the economic cost of illness and exposed a lack of health insurance among the elderly.
Rice was later the director of the National Center for Health Statistics from 1976 to 1982, where she helped create the National Death Index. She finished her career at the University of California, San Francisco, where she was a Regents' lecturer and professor emeritus. During her time at the university, she co-authored a paper on the costs of smoking, which impacted ongoing legal negotiations between the US government and the US tobacco industry and contributed to the Tobacco Master Settlement Agreement. (Full article...) -
Coffin birth, also known as postmortem fetal extrusion, is the expulsion of a nonviable fetus through the vaginal opening of the decomposing body of a deceased pregnant woman due to increasing pressure from intra-abdominal gases. This kind of postmortem delivery occurs very rarely during the decomposition of a body. The practice of chemical preservation, whereby chemical preservatives and disinfectant solutions are pumped into a body to replace natural body fluids (and the bacteria that reside therein), have made the occurrence of "coffin birth" so rare that the topic is rarely mentioned in international medical discourse.
Typically during the decomposition of a human body, naturally occurring bacteria in the organs of the abdominal cavity (such as the stomach and intestines) generate gases as by-products of metabolism, which causes the body to swell. In some cases, the confined pressure of the gases can squeeze the uterus (the womb), even forcing it downward, and it may turn inside-out and be forced out of the body through the vaginal opening (a process called prolapse). If a fetus is contained within the uterus, it could therefore be expelled from the mother's body through the vaginal opening when the uterus turns inside-out, in a process that, to outward appearances, mimics childbirth. The main differences lie in the state of the mother and fetus and the mechanism of delivery: in the event of natural, live childbirth, the mother's contractions thin and widen the cervix to expel the infant from the womb; in a case of coffin birth, built-up gas pressure within the putrefied body of a pregnant woman pushes the dead fetus from the body of the mother. (Full article...) -
Henoch–Schönlein purpura (HSP), also known as IgA vasculitis, is a disease of the skin, mucous membranes, and sometimes other organs that most commonly affects children. In the skin, the disease causes palpable purpura (small, raised areas of bleeding underneath the skin), often with joint pain and abdominal pain. With kidney involvement, there may be a loss of small amounts of blood and protein in the urine (hematuria and proteinuria), but this usually goes unnoticed; in a small proportion of cases, the kidney involvement proceeds to chronic kidney disease. HSP is often preceded by an infection, such as a throat infection.
HSP is a systemic vasculitis (inflammation of blood vessels) and is characterized by deposition of immune complexes containing the antibody immunoglobulin A (IgA); the exact cause for this phenomenon is unknown. In children, it usually resolves within several weeks and requires no treatment apart from symptom control but may relapse in a third of cases and cause irreversible kidney damage in about one in a hundred cases. In adults, the prognosis is different from in children. The average duration of cutaneous lesions is 27.9 months. For many, it tends to be relapsing–remitting over a long period of time, rather than self-limiting and there tend to be more complications. (Full article...) -
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea or shortness of breath, cough, sputum production and/or exacerbations) due to abnormalities of the airways (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.
The main symptoms of COPD include shortness of breath and a cough, which may or may not produce mucus. COPD progressively worsens, with everyday activities such as walking or dressing becoming difficult. While COPD is incurable, it is preventable and treatable. The two most common types of COPD are emphysema and chronic bronchitis and have been the two classic COPD phenotypes. However, this basic dogma has been challenged as varying degrees of co-existing emphysema, chronic bronchitis, and potentially significant vascular diseases have all been acknowledged in those with COPD, giving rise to the classification of other phenotypes or subtypes. (Full article...) -
Solar urticaria (SU) is a rare condition in which exposure to ultraviolet or UV radiation, or sometimes even visible light, induces a case of urticaria or hives that can appear in both covered and uncovered areas of the skin. It is classified as a type of physical urticaria. The classification of disease types is somewhat controversial. One classification system distinguished various types of SU based on the wavelength of the radiation that causes the breakout; another classification system is based on the type of allergen that initiates a breakout.
The agent in the human body responsible for the reaction to radiation, known as the photoallergen, has not yet been identified. The disease itself can be difficult to diagnose properly because it is so similar to other dermatological disorders, such as polymorphous light eruption or PLE. The most helpful test is a diagnostic phototest, a specialized test which confirms the presence of an abnormal sunburn reaction. Once recognized, treatment of the disease commonly involves the administration of antihistamines, and desensitization treatments such as phototherapy. In more extreme cases, the use of immunosuppressive drugs and even plasmapheresis may be considered. (Full article...) -
Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms.
The most common life-threatening concern with DVT is the potential for a clot to embolize (detach from the veins), travel as an embolus through the right side of the heart, and become lodged in a pulmonary artery that supplies blood to the lungs. This is called a pulmonary embolism (PE). DVT and PE comprise the cardiovascular disease of venous thromboembolism (VTE). About two-thirds of VTE manifests as DVT only, with one-third manifesting as PE with or without DVT. The most frequent long-term DVT complication is post-thrombotic syndrome, which can cause pain, swelling, a sensation of heaviness, itching, and in severe cases, ulcers. Recurrent VTE occurs in about 30% of those in the ten years following an initial VTE. (Full article...)
Did you know –
- ... that lagophthalmos is the inability to close the eyelids?
- ... that Beck's triad of arterial hypotension, raised jugular venous pressure and muffled heart sounds is pathognomonic of cardiac tamponade?
- ... that dark chocolate contains the highest antioxidant content of any food? It contains phosphorus, magnesium, iron and potassium. In addition, dark chocolate can lower blood pressure.
General images –
-
An American billing clerk preparing a detailed invoice. (1992) (from Medical billing)
-
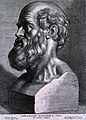
Emil Kraepelin (1856–1926), the founder of modern scientific psychiatry, psychopharmacology and psychiatric genetics. (from History of medicine)
-
Life expectancy vs healthcare spending of rich OECD countries. US average of $10,447 in 2018. (from Health care)
-
Jackson Memorial Hospital in Miami, the primary teaching hospital of the University of Miami's Miller School of Medicine and the largest hospital in the United States with 1,547 beds (from Health care)
-
The plinthios brochos as described by Greek physician Heraklas, a sling for binding a fractured jaw. These writings were preserved in one of Oribasius' collections. (from History of medicine)
-
Life Expectancy of the total population at birth among several OECD member nations. Data source: OECD's iLibrary (from Health insurance)
-
Seven named physicians and botanists of the Classical world from Vienna Dioscurides. Clockwise from top center: Galen, Dioscorides, Nicander, Rufus of Ephesus, Andreas of Carystus, Apollonius Mus or of Pergamon, Crateuas (from History of medicine)
-
Magical stela or cippus of Horus inscribed with healing encantations (c. 332 to 280 BCE). (from History of medicine)
-
Galen (129–216 CE), known for his wide insights into anatomy. (from History of medicine)
-
Yarrow, a medicinal plant found in human-occupied caves in the Upper Palaeolithic period. (from History of medicine)
-
"Diagram of the causes of mortality in the army in the East" by Florence Nightingale. (from History of medicine)
-
"More Doctors Smoke Camels than Any Other Cigarette" advertisement for Camel cigarettes in the 1940s (from Medical ethics)
-
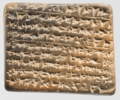
A Neo-Assyrian cuneiform tablet fragment describing medical text (c. 9th to 7th century BCE). (from History of medicine)
-
National Hospital for Neurology and Neurosurgery in London, United Kingdom is a specialist neurological hospital. (from Health care)
-
A 12th-century manuscript of the Hippocratic Oath in Greek, one of the most famous aspects of classical medicine that carried into later eras (from History of medicine)
-
The numbers of Americans lacking health insurance and the uninsured rate from 1987 to 2008 (from Health insurance)
-
Smallpox vaccination in Niger, 1969. A decade later, this was the first infectious disease to be eradicated. (from History of medicine)
-
Total healthcare cost per person. Public and private spending. US dollars PPP. For example: $6,319 for Canada in 2022. $12,555 for the US in 2022. (from Health care)
-
American combat surgery during the Pacific War, 1943 (from History of medicine)
-
A cuneiform terracotta tablet describing a medicinal recipe for poisoning (c. 18th century BCE). Discovered in Nippur, Iraq.
-
Mandrake (written 'ΜΑΝΔΡΑΓΟΡΑ' in Greek capitals). Naples Dioscurides, 7th century (from History of medicine)
-
Hippocrates (c. 460–370 BCE). Known as the "father of medicine". (from History of medicine)
-
Curandera performing a limpieza in Cuenca, Ecuador (from Traditional medicine)
-
Patient, Surrey County Lunatic Asylum, c. 1850–58. The asylum population in England and Wales rose from 1,027 in 1827 to 74,004 in 1900. (from History of medicine)
-
Botánicas such as this one in Jamaica Plain, Boston, cater to the Latino community and sell folk medicine alongside statues of saints, candles decorated with prayers, lucky bamboo, and other items. (from Traditional medicine)
-
Mexico City epidemic of 1737, with elites calling on the Virgin of Guadalupe (from History of medicine)
-
healthcare expenditure in Japan by age group (from Health insurance)
-
Statue of Robert Koch, father of medical bacteriology, at Robert-Koch-Platz (Robert Koch square) in Berlin (from History of medicine)
-
Sketch of Muslim physician Muhammad ibn Zakariya al-Razi (from History of medicine)
-
AMA Code of Medical Ethics (from Medical ethics)
-
A Ukrainian monument to the HIV pandemic. (from History of medicine)
-
Charite in Berlin (from History of medicine)
-
Medical personnel place sterilized covers on the arms of the daVinci Xi surgical system, a minimally-invasive robotic surgery system, at the William Beaumont Army Medical Center. (from History of medicine)
-
Sometimes traditional medicines include parts of endangered species, such as the slow loris in Southeast Asia. (from Traditional medicine)
-
Infographic showing how healthcare data flows within the billing process (from Medical billing)
-
Medicine during the First World War - Medical Transport. (from History of medicine)
-
COVID-19 swab testing in Rwanda (2021). (from History of medicine)
-
Taoist symbol of Yin and Yang (from Medical ethics)
-
Guy's Hospital in 1820 (from History of medicine)
-
Health spending by country. Percent of GDP (Gross domestic product). For example: 11.2% for Canada in 2022. 16.6% for the United States in 2022. (from Health care)
-
Global concentrations of health care resources, as depicted by the number of physicians per 10,000 individuals, by country. Data is sourced from a World Health Statistics 2010, a WHO report.[needs update] (from Health care)
-
Ethical prayer for medical wisdom by Dr Edmond Fernandes (from Medical ethics)
-
The emergency room is often a frontline venue for the delivery of primary medical care. (from Health care)
-
Zhang Zhongjing – a Chinese pharmacologist, physician, inventor, and writer of the Eastern Han dynasty. (from History of medicine)
-
Primary care may be provided in community health centers. (from Health care)
-
18th-century medical remedies collected by a British Gentry family (from History of medicine)
-
The Edwin Smith Surgical Papyrus, written in the 17th century BCE, contains the earliest recorded reference to the brain. New York Academy of Medicine. (from History of medicine)
-
Most countries have seen a tremendous increase in life expectancy since 1945. However, in southern Africa, the HIV epidemic beginning around 1990 has eroded national health. (from History of medicine)
-
The Quaker-run York Retreat, founded in 1796, gained international prominence as a centre for moral treatment and a model of asylum reform following the publication of Samuel Tuke's Description of the Retreat (1813). (from History of medicine)
-
Depiction of smallpox in Franciscan Bernardino de Sahagún's history of the conquest of Mexico, Book XII of the Florentine Codex, from the defeated Aztecs' point of view (from History of medicine)
-
Health Expenditure per capita (in PPP-adjusted US$) among several OECD member nations. Data source: OECD's iLibrary (from Health insurance)
-
A doctor checks a patient's pulse in Meiji-era Japan. (from History of medicine)
-
A cochlear implant is a common kind of neural prosthesis, a device replacing part of the human nervous system. (from History of medicine)
More Did you know (auto generated)

- ... that Tang Zonghai was one of the first advocates for the integration of Chinese and Western medicine?
- ... that Margaret C. Roberts was encouraged to study medicine by LDS Church leader Brigham Young to reduce mortality rates during childbirth?
- ... that a lack of screening for pregnant women with syphilis in sub-Saharan Africa is associated with increased infant mortality?
- ... that fourteenth-century Buddhist monk Tuệ Tĩnh is referred to as a founding father of traditional Vietnamese medicine?
- ... that Indian gynaecologist and reproductive medicine pioneer Baidyanath Chakrabarty, who performed over 4,000 IVF procedures, was a cricket fan who thought Virat Kohli and Ashwin were "such good boys"?
- ... that the Noongar used the Eucalyptus wandoo tree as a medicine and ointment?
Topics
Categories
Recognized content
Associated Wikimedia
The following Wikimedia Foundation sister projects provide more on this subject:
-
Commons
Free media repository -
Wikibooks
Free textbooks and manuals -
Wikidata
Free knowledge base -
Wikinews
Free-content news -
Wikiquote
Collection of quotations -
Wikisource
Free-content library -
Wikiversity
Free learning tools -
Wiktionary
Dictionary and thesaurus



























































![Image 46Global concentrations of health care resources, as depicted by the number of physicians per 10,000 individuals, by country. Data is sourced from a World Health Statistics 2010, a WHO report.[needs update] (from Health care)](http://upload.wikimedia.org/wikipedia/commons/thumb/1/1f/Global_physician_density_map_-_WHO_2010.png/120px-Global_physician_density_map_-_WHO_2010.png)