Search results
Appearance
There is a page named "Confusion Assessment Method" on Wikipedia
- The Confusion Assessment Method (CAM) is a diagnostic tool developed to allow physicians and nurses to identify delirium in the healthcare setting. It...23 KB (1,548 words) - 05:32, 18 December 2023
- Delirium (redirect from Acute confusion)Siegal AP, Horwitz RI (December 1990). "Clarifying confusion: the confusion assessment method. A new method for detection of delirium". Annals of Internal...98 KB (10,735 words) - 10:51, 28 February 2025
- learning and specifically the problem of statistical classification, a confusion matrix, also known as error matrix, is a specific table layout that allows...15 KB (1,665 words) - 14:19, 28 February 2025
- a validated clinical tool. The two most widely used are the Confusion Assessment Method for the ICU (CAM-ICU) and the Intensive Care Delirium Screening...22 KB (1,820 words) - 07:04, 24 January 2025
- Obtaining a RASS score is the first step in administering the Confusion Assessment Method in the ICU (CAM-ICU), a tool to detect delirium in intensive...5 KB (464 words) - 21:13, 26 February 2024
- 4AT (category Mental disorders screening and assessment tools)diagnostic randomized controlled trial comparing the 4AT and the Confusion Assessment Method (CAM) found that the 4AT had higher sensitivity and similar specificity...32 KB (3,106 words) - 10:23, 15 November 2024
- Horwitz, R. I. (December 15, 1990). "Clarifying confusion: the confusion assessment method. A new method for detection of delirium". Annals of Internal...13 KB (1,299 words) - 20:22, 23 September 2024
- anesthesia in the PACU were assessed for delirium using the Confusion Assessment Method for the ICU (CAM-ICU) found rates of emergence delirium of 31%...10 KB (1,001 words) - 19:03, 27 March 2024
- The scientific method is an empirical method for acquiring knowledge that has been referred to while doing science since at least the 17th century. Historically...198 KB (23,337 words) - 17:11, 3 March 2025
- Health technology assessment (HTA) is a multidisciplinary process that uses systematic and explicit methods to evaluate the properties and effects of...15 KB (1,530 words) - 06:58, 12 January 2025
- outcomes as concussions without convulsions. Cognitive symptoms include confusion, disorientation, and difficulty focusing attention. Loss of consciousness...118 KB (12,247 words) - 15:34, 14 March 2025
- transparent and repeatable method), some academic publishers categorize them as a kind of 'systematic review', which may cause confusion. Scoping reviews are...83 KB (9,042 words) - 07:30, 22 January 2025
- SOAP note (redirect from Subjective Objective Assessment Plan)The SOAP note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out...16 KB (1,762 words) - 03:02, 14 February 2025
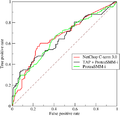
- prediction result or instance of a confusion matrix represents one point in the ROC space. The best possible prediction method would yield a point in the upper...61 KB (7,870 words) - 16:28, 3 March 2025
- also requires students to learn how to articulate their confusion, a useful skill. This method is effective in courses that call for problem-solving. Students...10 KB (1,275 words) - 01:25, 25 March 2024
- The Tinetti Test (TT), or Performance Oriented Mobility Assessment (POMA), is a common clinical test for assessing a person's static and dynamic balance...3 KB (241 words) - 20:00, 13 May 2024
- Post-traumatic amnesia (redirect from Posttraumatic confusional state)of the method most often used in assessing PTA, the Galveston Orientation and Amnesia Test (GOAT), is that it does not include any assessment of attention...57 KB (7,467 words) - 09:12, 3 March 2024
- of using this assessment include the simplicity of administration and ease of participant understanding. Another feature of the assessment that is notable...6 KB (776 words) - 03:01, 12 June 2024
- by the presence of high carbon dioxide concentrations in the blood. This method also makes the direct cause of death difficult to trace if the bag and gas...34 KB (3,935 words) - 17:47, 17 March 2025
- to think, headaches, nausea, and poor balance. Severe symptoms include confusion, seizures, and coma; death can ensue. The causes of hyponatremia are typically...39 KB (4,316 words) - 14:02, 13 November 2024
- the same area, on different assessments, with different deductions and by different collectors, has produced great confusion and expense; and that in any
- initially assessed at age 20 and again as civilians at age 35. The initial assessment included a psychiatric interview, objective indicators of conscript competence
- students multiple choice questions is one method of assessment. In chapter 2, article 1, of _Foundations and Assessment_, the author discusses a number of other