Essure: Difference between revisions
→Cautions and warnings: remove errant fact tag |
insert controversy into lead - making global news, can't really miss it now |
||
| Line 26: | Line 26: | ||
Two economic studies, one of which implemented Essure as an in-office procedure, suggest that Essure could be more cost-effective than [[laparoscope|laparoscopic]] bilateral [[tubal ligation]].<ref name=Hurskainen/> |
Two economic studies, one of which implemented Essure as an in-office procedure, suggest that Essure could be more cost-effective than [[laparoscope|laparoscopic]] bilateral [[tubal ligation]].<ref name=Hurskainen/> |
||
Since 2013, the product has been the subject of controversy with women complaining of severe side effects leading to surgical extraction,<ref name=CT20131222/> and campaigner [[Erin Brockovich]] hosting a website where women can share their stories after having the procedure.<ref name=CT20131222/><ref name=BBC27871265/> |
|||
==Procedure== |
==Procedure== |
||
Revision as of 13:10, 24 June 2014
| Essure | |
|---|---|
| Background | |
| Type | Sterilization |
| First use | 2002 |
| Failure rates (first year, after occlusion) | |
| Perfect use | 0.26% |
| Typical use | 0.26% |
| Usage | |
| Duration effect | Permanent |
| Reversibility | Irreversible |
| User reminders | Additional methods until 3 month check by hysterosalpingogram |
| Clinic review | None |
| Advantages and disadvantages | |
| STI protection | No |
| Benefits | Permanent contraception |
Essure is a permanent, non-surgical transcervical sterilization procedure for women developed by Conceptus Inc., a fully-owned subsidiary of Bayer AG of Germany since June 5, 2013.[1] It was approved for use in the United States on November 4, 2002.[2]
Two economic studies, one of which implemented Essure as an in-office procedure, suggest that Essure could be more cost-effective than laparoscopic bilateral tubal ligation.[3]
Since 2013, the product has been the subject of controversy with women complaining of severe side effects leading to surgical extraction,[4] and campaigner Erin Brockovich hosting a website where women can share their stories after having the procedure.[4][5]
Procedure
The procedure takes about 10 minutes,[citation needed] for a trained physician to perform and can be performed in a physician's office.[citation needed] General anesthesia is not required.[6]
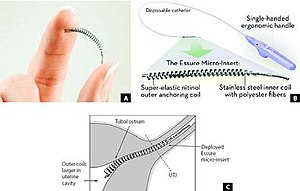
Small, flexible inserts are placed into the fallopian tubes by a catheter passed from the vagina through the cervix and uterus.[citation needed] The insert contains inner polyethylene terephthalate fibers to induce benign fibrotic reaction and is held in place by flexible stainless steel inner coil and a dynamic outer nickel titanium alloy coil.[7] Once in place, the device is designed to elicit tissue growth in and around the insert over a period of three months to form an occlusion or blockage in the fallopian tubes; the tissue barrier formed prevents sperm from reaching an egg.[citation needed]
Unlike other forms of tubal ligation, no general anaesthetic nor incision through the abdomen is required.[citation needed] Similar to some other methods of birth control, initially additional forms of birth control must be continued for 3 months[3] to prevent pregnancy until the method's effectiveness can be confirmed.
Follow-up
For the Essure method, three months after insertion a Radiologist physician performs an x-ray procedure called a hysterosalpingogram,[8] to confirm that the fallopian tubes are completely blocked and that the patient can rely on the Essure inserts for birth control.[2] A contrast agent (dye) is injected through the cervix, and an x-ray technologist takes photos of the Essure coils to ensure no contrast leaks past the Essure.
Efficacy
Following successful insertion and occlusional response, the Essure procedure is 99.74% effective based on 5 years of follow-up.[9][10]
The reported insertional failure rates are "failure to place 2 inserts in the first procedure (5%), initial tubal patency (3.5%), expulsion (2.2%), perforation (1.8%), or other unsatisfactory device location (0.6%)".[11] Upon follow-up, occlusion is observed to have occurred in 96.5% of patients at 3 months with the remainder occluded by 6 months.[2]
Cautions and warnings
The inserts are made from polyester fibers, nickel-titanium and stainless steel and solder and are safe to use with MRI equipment. Unlike many temporary methods of birth control, the Essure inserts do not contain or release hormones. The inserts do not prevent the transmission of sexually transmitted diseases.
The procedure is reported to be permanent and not reversible by the manufacturing company. Notwithstanding the manufacturer's position, several Essure reversals have been performed.[12]
Additional birth control must be used for three months after procedure.[11][13]
Risks
- Perforation, expulsion, or other unsatisfactory location of the insert
- Pregnancy and increased risk of ectopic pregnancy
- Pain, cramping, vaginal bleeding, menstrual pattern changes, light periods at first then longer, heavier periods lasting up to 6–8 weeks due to changing birth control methods to a non-hormonal solution
- Nausea/vomiting
- Vasovagal response (fainting)
- Allergic reaction to the materials
- Heightened allergic response to other allergens
- heavy metal toxicity
- itchy, raised rash
- brain fog
- autoimmune disease symptoms
- weight gain
- anxiety/depression
- hair loss
Controversy
In 2013, the product made news in North America, with women complaining of severe side effects leading to surgical extraction. According to one article, women who have gotten pregnant are naming these children e-babies.[4]
The FDA released a statement on October 25 2013, stating that since the product was approved in 2002 that it had received 943 reports of adverse events related to Essure, mainly for pain (606 of the complaints).[5] An additional 1,000 more complaints have been sent to the FDA in a voluntary reporting system, but physicians are not obliged to report complaints.[5]
A Facebook group called Essure Problems has 8,592 members who call the method "E-hell" and mostly complain about pain, bleeding and bloating from the device. Some say they've had coils break and perforate their internal organs.[5] Erin Brockovich hosts a website where women can share their stories after having the procedure.[4][5]
References
- ^ "Essure Permanent Birth Control". U.S. Food and Drug Administration. Retrieved June 24, 2014.
- ^ a b c "Essure[[Trademark|™]] System - P020014". US Food and Drug Administration. 2009-06-29. Retrieved 2011-05-21.
{{cite web}}: URL–wikilink conflict (help) - ^ a b Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1016/j.fertnstert.2009.02.080, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1016/j.fertnstert.2009.02.080instead. - ^ a b c d "Women report complicatidiseasesons from Essure birth control". Chicago Tribune. Retrieved March 2, 2014.
- ^ a b c d e Regan Morris (June 24, 2014). "Erin Brockovich calls for end to Bayer's Essure". BBC News, Los Angeles. Retrieved June 24, 2014.
- ^ http://www.marketwatch.com/story/conceptusr-to-promote-gynecare-thermachoicer-to-us-physician-offices-2010-11-10?reflink=MW_news_stmp
- ^ Miño M, Arjona JE, Cordón J, Pelegrin B, Povedano B, Chacon E. Success rate and patient satisfaction with the Essure sterilisation in an outpatient setting: a prospective study of 857 women. BJOG. 2007 Jun;114(6):763-6.
- ^ "Essure Confirmation Test". Conceptus Inc. Retrieved 2011-05-30.
- ^ control methodsbyConceptus/Understanding/ClinicalTesting/tabid/58/Default.aspx "Clinical Testing". Essure. Conceptus. Retrieved 2006-12-12.
{{cite web}}: Check|url=value (help) [dead link] - ^ Smith RD (January 2010). "Contemporary hysteroscopic methods for female sterilization". Int J Gynaecol Obstet. 108 (1): 79–84. doi:10.1016/j.ijgo.2009.07.026. PMID 19716128.
- ^ a b "Prescribing Information" (PDF). Essure. Conceptus. 2005-09-08. Archived from the original (PDF) on 2006-11-11. Retrieved 2006-12-12.
- ^ "Doctors Confirm First Successful Essure Tubal Ligation Reversal". 2008-10-08. Retrieved 2010-02-15., referring to Dr. William A.C. Greene Jr. and Dr. Wendell Turner at Lakeshore Surgical Center
- ^ Hurskainen R, Hovi SL, Gissler M; et al. (April 2009). "Hysteroscopic tubal sterilization: a systematic review of the Essure system". Fertil. Steril. 94 (1): 16–19. doi:10.1016/j.fertnstert.2009.02.080. PMID 19409549.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link)
External links
